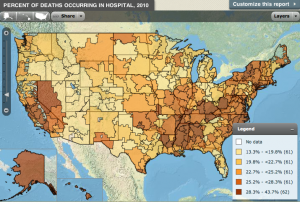
A recent article from Health Leaders Media discusses a Dartmouth Atlas report which finds that even though the cost of intensive hospice/hospital care is on the rise, that “aggressive end-of-life care” is in decline. And it is the rapidity of this transition that has stunned doctors most. “Patients dying in 2010,” states the report, “were less likely to spend a portion of their last days in a hospital, and were less likely to die in one than in 2007.” The report states that the Hershey Medical Center in Hershey, PA saw a “26% reduction rate in ICU days over a three year period and an 18% reduction in physician visits.”
“This [reduction] does not happen by accident,” explains the co-principal investigator of the Dartmouth Atlas Project, David Goodman, MD.
Meanwhile, the average spending for a terminally ill Medicare patient increased 15.2% in the last two years of life, “from $60,694 in 2007 to $69,947 in 2010.” While the costs were “not adjusted for inflation,” Goodman states that the rise was far higher than the consumer price index of 5.2%.
“Whether we’re beating the cost of living index or lagging behind, the norm is what’s killing us,” he states, “[and] there’s strong evidence that lengthy end-of-life stays in hospitals and receiving uncomfortable procedures are not what patients want.” And after studying the progression of end-of-life care in hospitals in around 18 states, the report found that “practices to encourage more appropriate care for terminally ill patients has stagnated” overall.
The report itself is based in observations of “various healthcare services at the end of life such as time spent in a hospital, [the] number of physician visits, durable medical equipment, and whether the patient died during a hospital stay.”
Goodman states that some of the blame for the decline can be placed on doctors and clinicians who are simply “not very good at assessing patient preferences. [They] don’t receive the training to do it. Aggressive care [is] making good on a pledge to extend [a] life [by] a week or a month longer. Too often these discussions never occur.”
You may also be interested in:
- TIME’s Joe Klein Talks End-of-Life Care in His Article “The Long Goodbye”
- Vermont Passes Aid-in-Dying Legislation
- 10 Facts About Hospice Care You May Not Know

 Dartmouth Report Says “Agressive End-of-Life Care” is in Decline
Dartmouth Report Says “Agressive End-of-Life Care” is in Decline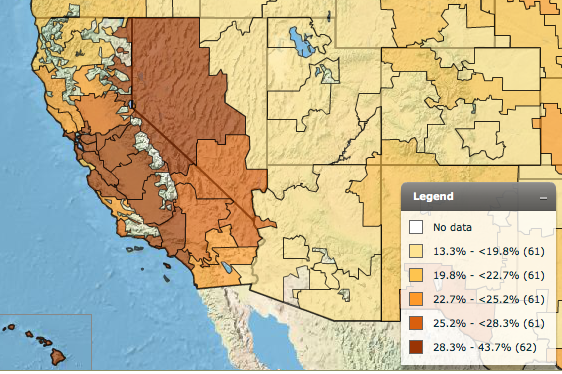



 Meaning-Focused Grief Therapy: Imaginal Dialogues with the Deceased
Meaning-Focused Grief Therapy: Imaginal Dialogues with the Deceased
















