
Credit: dailymail.co.uk
Scientists have long known that there is a strong correlation between diabetes and dementia, particularly Alzheimer’s disease. People living with diabetes have an incidence of Alzheimer’s that is roughly twice that of the general population, and they tend to show signs of cognitive decline at an earlier age. Until recently, however, no one was sure why this was the case.
Now, a growing body of research is pointing to high blood sugar levels as a key factor in the development of diabetes-related dementia. Moreover, insulin resistance — which occurs when blood sugar is high over a prolonged period of time — appears to be closely linked to both declining brain function and the development of Alzheimer’s characteristic amyloid plaques.
Type 1 and Type 2 Diabetes
For a long time, doctors have believed that there are two types of diabetes, Type 1 and Type 2. Type 1 diabetes is an autoimmune disorder in which the body’s immune system destroys the cells in the pancreas that produce insulin, a hormone that helps move glucose into the cells. Glucose, a simple sugar derived from dietary sources, provides the body with energy: Without it, cells cannot support metabolism and eventually die.
Unlike Type 1 diabetes, in which insulin levels are too low, in Type 2 diabetes, insulin levels are too high.
Type 2 diabetes occurs when the insulin-producing cells in the pancreas are exposed to high levels of glucose over an extended period of time; as a result, they are forced to pump out more and more insulin to “keep up” with the demand. Unlike Type 1 diabetes, in which insulin levels are too low, in Type 2 diabetes, insulin levels are too high. Because of this, all of the cells in the body eventually develop what’s called “insulin resistance.” That is, they stop letting insulin do its job.
Because the cells in the brain need a great deal of energy, they are some of the first to die.
The net result in both diseases is that all of the cells in the body are deprived of glucose and begin to slowly “starve to death.” Because the cells in the brain need a great deal of energy (and glucose) they are some of the first to die. Scientists believe this is a major reason why people with diabetes experience early and significant cognitive decline.
What Is Type 3 Diabetes?
Over the past decade, scientists have discovered that insulin is not only produced in the pancreas; it is also made in the brain. Moreover, they have found that this “brain insulin” does more than just help transport glucose into the cells. It also has a very important function in the creation of neurotransmitters — chemicals that help move impulses between nerve cells. Insulin is also essential to many of the neurocognitive functions involved in learning and memory.
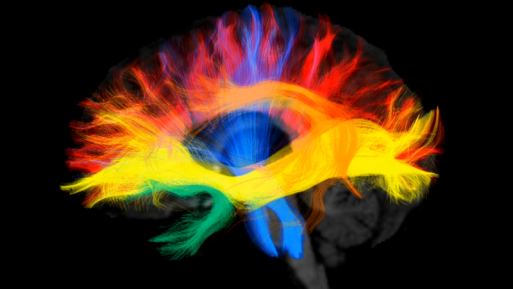
The brain depends on insulin to function properly
(Credit: pbs.org)
Based on these findings, many researchers have come to believe that the cognitive decline seen in people with diabetes is closely associated with insulin resistance in the brain. Hence, the term Type 3 diabetes, or “brain diabetes” was born.
Interestingly, there is also a growing body of evidence linking insulin resistance and beta-amyloids, the substances believed to be responsible for the plaques found in the brains of people with Alzheimer’s disease. The mechanism by which the two intersect, however, is poorly understood. Some studies suggest that beta-amyloids enhance insulin resistance, thereby contributing to cognitive decline. Others suggest that insulin resistance aids in the creation of the amyloid plaques and tangles that contribute to the symptoms of Alzheimer’s disease.
There is also evidence that an underlying biochemical mechanism, perhaps with a genetic link, contributes to both.
Treatment Implications
The link between insulin resistance and Alzheimer’s disease presents intriguing possibilities for treatment of dementia and cognitive decline. For example, a number of studies have shown that administering insulin intranasally (a route that enhances absorption in the brain) improves cognitive function in both healthy volunteers and people with Alzheimer’s disease.
Additionally, a class of medications known as glucagon-like peptide 1 receptor agonists have been shown to both decrease insulin resistance and improve cognition, memory and cell survival in the brain. Two of these medications, exenatide (Byetta, Bydureon) and liraglutide (Victoza) have already been approved for use in Type 2 diabetes and are undergoing preclinical trials for the treatment of Alzheimer’s disease.
Prevention Is the Best Cure

Credit: livewellmagazine.org
Not all cases of Alzheimer’s disease and dementia are linked to insulin resistance and Type 2 diabetes. However, it is clear that preventing the onset of Type 2 diabetes is an important step in staving off cognitive decline.
According to the National Institute of Diabetes and Digestive and Kidney Diseases, the best way to prevent Type 2 diabetes is to follow a healthy lifestyle: Eat right; stop smoking; exercise regularly; lower your stress level; and maintain a healthy weight. Cutting down on or eliminating sugar in your diet also significantly helps decrease diabetes risk, a recent Stanford University study shows.

 Is Alzheimer’s Disease Type 3 Diabetes?
Is Alzheimer’s Disease Type 3 Diabetes?


 Final Messages of the Dying
Final Messages of the Dying
 Will I Die in Pain?
Will I Die in Pain?















