This is an interview with an oncologist at a leading cancer treatment center in Tucson, Arizona. We will call him Doctor C.
Aurora: What question do you most often receive as an oncologist?
Dr. C: “How do you stand it?” Which is a very hard question to answer, surprisingly. I don’t really know the answer. Like everyone else, I suffer along with my patients. But I manage to not let it ruin my life. I’m usually able to walk away at the end of the day and come home to a different world.
Aurora: What makes a good doctor?
Dr. C: Well I can tell you what makes a bad doctor — Every time a doctor walks into an Intensive Care Unit (ICU) to see a patient, he can charge $100 or more just to pick up a chart and write “no change.” Even if the person in an ICU has terminal cancer, is intubated on a breathing machine, and on pressor amines (chemicals that keep blood pressure artificially raised). In other words, it’s useless and futile and all you’re dong is prolonging a meaningless existence for someone who’s comatose and effectively already dead. I find this shockingly immoral.
This is often justified by the claim that the desperate family is begging the doctor to do anything to extend the life of their loved one as long as possible — but as a doctor, you don’t have to do this. If you’re caught in a situation where the family is hysterical and asking you to keep your patient technically alive, hospitals have ethics committees to determine when it serves no purpose. Meanwhile, the hospital bill continues to escalate, so the hospitals aren’t really opposed to this practice. Insurance companies have to pay more to doctors, and as a result, insurance premiums rise. It benefits no one.
Aurora: Well doctor, you didn’t really answer my question, but I think I have a better one: how do we avoid this happening to us, or someone we love?
Dr. C: You make a living will, where you specify no extreme measures. In particular, there are two orders you can implement at the end of life: DNI and DNR, do not intubate, and do not resuscitate. In other words, if I’m dying, let me go. Of course you should only implement these orders if you’re suffering from a terminal disease. Or you can put these decisions into the hands of someone you trust.
Aurora: How do you feel about aid in dying?
Dr. C: I’m altogether in favor of it. I think that whenever a patient says, “I’ve really had it, can you help me along?” your answer should always be, “yes, I will help you.” But because it’s illegal, you have to lie and cheat and finagle and fudge the chart. You have to say in your progress notes: “patient in terrible pain, have to increase morphine on hourly basis to treat severe pain.” Morphine suppresses respiration, causing pneumonia, which you are under no obligation to treat. Active euthanasia and withholding treatment are different in the eyes of the law.
Aurora: What advice do you have for cancer patients?
Dr. C: The best advice I would have for a new cancer patient who needs an oncologist is to find one that you like, not necessarily the one most highly recommended or with the highest academic credentials. Find someone who you feel likes you and wants to help you. This is of course true of doctors in general.
Lastly, you have the right to die at home. You shouldn’t let doctors or family members browbeat you into coming into the hospital for terminal care. People are less frightened and more comfortable at home. Also, remember hospice care is available.
Aurora: Thanks so much, doc!
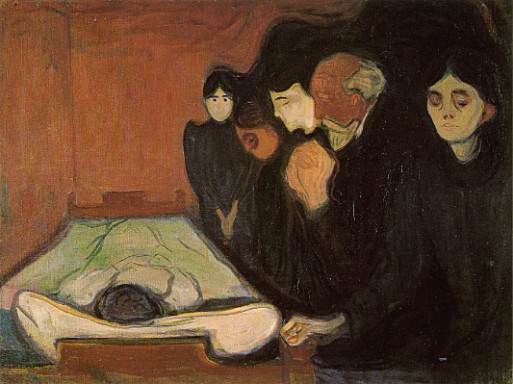
Image Source: edvard-munch.com

 What are some advice for cancer patients? An Interview with Doctor C
What are some advice for cancer patients? An Interview with Doctor C


 Final Messages of the Dying
Final Messages of the Dying
 Will I Die in Pain?
Will I Die in Pain?















