Today Sevenponds speaks with Dress Wedding, a Holistic Services Director with Harborside Health Center located in Oakland, California. Also joining Dress is Kelly Quirke, Community Engagement Coordinator. This is the first part of a two-part interview with Harborside, a state-of-the-art medical marijuana dispensary in Oakland and San Jose, California. Dress and Kelly offered me a walking tour of the surprisingly large cannabis dispensary, while we discussed the emerging acceptance of medical marijuana and how cannabis helps those at end of life.
Note: This interview has been edited for length and clarity.
 Suzette Sherman: [As we stand at the Haborside Health Center interior entrance area] Thanks for giving me a tour so our readers can better understand how cannabis can help those at the end of life.
Suzette Sherman: [As we stand at the Haborside Health Center interior entrance area] Thanks for giving me a tour so our readers can better understand how cannabis can help those at the end of life.
Dress Wedding: Of course. Let’s start at the entrance. We always have someone here at the entry door checking to be sure each person who walks in has a medical marijuana card. The card must be issued by a licensed-physician who can recommend medical marijuana for a variety of medical conditions. This room over here to the right is where we check to be sure it’s a legitimate card. (Sometimes we may make a call to the physician, if needed.) Patients check in and then log in. This front area over here is our community area.
Suzette: Wow, it looks like a beautifully designed contemporary store! I am surprised at what a large space this is. [We stand looking into the sales area and a lot of people are in line and looking at the cases of product.]
Dress: We are in a constant state of refining the process of getting patients through the dispensary. Over here we have our Healing Center. We have a staff of practitioners about 50 hours a week who provide a variety of holistic services. Would you like to look at the book?
Suzette: Absolutely.
Dress: We offer “Alexander Technique,” a “Grow Your Own Cannabis” class, a “Senior Citizen Cancer Support Group…”
Suzette: What happens at that support group?
Dress: It’s peer counseling. People share their experiences using different forms and varieties of cannabis. They describe the product, talk about best use scenarios and how it’s working for them. They also talk about any challenges they are having. For example, they may discuss how someone’s family is reacting, or whether they are feeling isolated. Then they are able to see what works and how to improve their treatments. We also have reiki, acupuncture, an herbalist and a chiropractor.
We have struggled with the stigma of cannabis use, and we are always trying to heal that and present ourselves in a responsible light. [Harborside’s owner Andrew Deangelo walks over.]
Dress: This is Andrew Deangelo.
Suzette: Hi Andrew. I’m Suzette Sherman with SevenPonds. SevenPonds is an online magazine that specializes in end of life.
Andrew Deangelo: My parents were greatly helped by cannabis at end of life, both my mom and my dad.
Suzette: They were?
Andrew: My dad was on the east coast, it was more problematic.
Suzette: You mean because of his location and access to cannabis?
Andrew: (He nods) Luckily I was in a position to do whatever was necessary to accommodate his needs.
Suzette: How long did your parents use cannabis?
Andrew: Both of them were already using cannabis as seniors for pain and pain management. When they were in hospice, they used it for spiritual and emotional healing as well. My mom had dementia so it was hard to have conversations. With my dad we used cannabis to facilitate cycle of life conversations. My dad did not talk easily…
Suzette: You mean about death.
Andrew: Yes.
Suzette: Men often have a more difficult time having that conversation.
Andrew: The cannabis was helpful. They were in their 80’s, an average age to die. My dad was three months in hospice. He suffered from depression because his second wife died a few years before. At night he was alone, and he couldn’t get away from that loneliness. Cannabis can help but there’s a downside because it’s still not being accepted in the United States. We try to take “village” approach here at Harborside, so people feel more comfortable using cannabis to help themselves feel better.
Sorry, I need to run now.
Suzette: It was really nice meeting you Andrew. [I follow Dress as he walks into the sales area.]
Dress: When we opened Harborside, we chose clear windows so people could see in. The staff were concerned, but we have not had any problems. Our tag line is “Out of the shadows, into the light.” Harborside Health Center broke the old model from stoner to healthcare. We don’t want our patients to feel like they’re walking into a jail with some tattooed guy helping them. We want patients to feel safe and secure. We get long lines of patients, and we work hard to engage them and encourage them to talk about what they are looking for. Many people know what they want, but others come seeking consultation.
We now have a consultation area for our staff to write suggestions down. We also work to have beautiful product placement. This is a lightly attended day today.
Suzette: Really, there’s a lot of people.
Dress: We just revamped our floor four months ago. It used to be that all of the patients were at the sales bar. Now the floor is separated into two areas: the sales bar and the consultation area, where patients can download what they’re looking for and see what the best choices are from the menu today. Our consulting staff advises them based on the experiences of our patients.
We have the largest quantity and selection of cannabis products in the world. We have deliveries two days a week, and we used to get long lines on those days. I would arrive here at 8 in the morning, and people would be here waiting for the doors to open at 9. There started to be tension among the people waiting outside, so we started a policy where people could call ahead for certain items that only come in on a limited basis.
Suzette: Who uses medical marijuana?
Dress: Nationally, seniors are the largest group of users. They typically use it for pain and appetite issues.
Suzette: Pain and appetite issues are typical for those at end of life. Although once you go into active dying your body naturally shuts down your need for food.
By the way, I just had dinner with a physician at Kaiser Medical Center who mentioned that Kaiser currently does not provide physician training for recommending marijuana to patients. Is this typical?
Dress: That’s not accurate. We work with hospice physicians at Kaiser.
Suzette: Sorry, she is not with hospice.
Dress: Well, yes, then. Not all doctors are fully trained in cannabis there, but the ones who work with hospice are knowledgeable. It is a “CYA” [cover your ass] issue for many physicians. They say they won’t recommend it, but they know the patient is using it.
My wife has health issues. She uses a tincture (alcohol-based cannabis extract in a bottle) to fall asleep. It was also preventing seizures. It took her physician quite some time to realize the cannabis was working better for her seizures than the medications he would recommend.
This concludes part one of my interview with Dress Wedding and Kelly Quirke. Please come back next week for part two of our interview, when we discuss more details about cannabis at end of life.

 How Can Cannabis Help Those at the End of Life?
How Can Cannabis Help Those at the End of Life?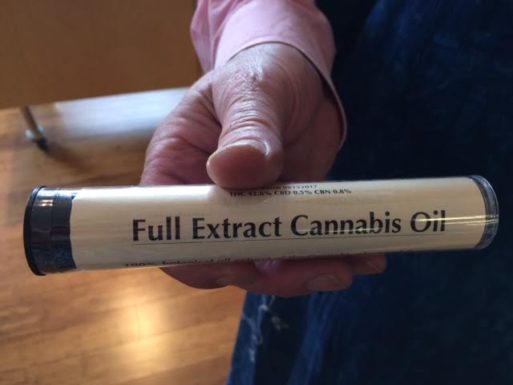





 Final Messages of the Dying
Final Messages of the Dying
 Will I Die in Pain?
Will I Die in Pain?















