Gayle MacDonald is a pioneer in oncology massage and its education. When she first began in 1993, massage therapists in training were instructed to avoid working with cancer patients altogether, because of the myth that massage would help “spread” cancer. Since then, Gayle has been at the forefront of developing standards of practice for hospitalized patients, so that anyone – whether they are affected by cancer, or in a later stage of dying – can safely benefit from the therapeutic power of touch.
Gayle got her start at Oregon Health and Science University in Portland, Oregon. After her own massage training, she quickly found her place as an educator, teaching and supervising other massage therapists to help patients on all levels of the cancer treatment spectrum. One of the founders of Oncology Massage Education Associates, Gayle has also authored three books on the topic of specialized massage.
“No matter what treatments a person is receiving or has received, they can benefit from touch therapy if certain adjustments are made. Skilled touch can be given at every state of the cancer experience. Massage given with care has the capacity to open hearts, create wholeness, and change lives. Conventional oncology treatments may cure the disease, but massage helps people connect with healing.” -Excerpt from “Medicine Hands: Massage Therapy for People with Cancer,” (3rd Ed.) (2014, Findhorn Press)
Her hope is that the practical knowledge and research she and her colleagues have contributed to the field of oncology massage will become a part of the core curriculum during standard massage therapy training. Gayle, now retiring after 28 years, has left an indelible mark on the world of touch. We were lucky to sit down with Gayle and hear some juicy tidbits from her decades of working to bring comfort and healing to those most needing it.
Editor’s note: This interview has been edited for length and clarity.
How did this work all begin for you?
One day I just happened to be at school – and at that time, I was never at school, because when you do an extern program you’re out in the field. The teaching and research hospital in Portland called and left a message for me. They wanted to know if I could bring our students to work with their cancer patients.
Were you prepared to work with those affected by cancer?
At that time, we were taught that you can’t touch cancer patients because of the fear that massage would move the cancer cells and the cancer would metastasize. They taught us not to touch cancer patients unless they were dying. But now we know that cancer starts and spreads because of genes mutating, and massage does not cause genes to mutate.
How did you tailor the standard massage for cancer patients?
I had to figure it out and just start from scratch. They assigned me a nurse mentor and she gave me some rules: if it’s painful do this, if it’s red then do this, but she didn’t tell me really everything I needed to know. I’m also inherently a very gentle person, which is a good fit.
Can you tell me about the first oncology massage you ever gave?
I remember the first person I worked with. He had had a bone marrow transplant about three weeks previous, and his platelet count was 36, which is desperately low, but it had no meaning to me yet. I probably used moderate pressure, but then I got home and figured out what a platelet count of 36 meant – I was petrified! I called my nurse contact, and she just kind of laughed, she says “they’re more resilient than then you know.”

Gentle touch comforts a cancer patient receiving a chemotherapy infusion
What did you learn about adjusting for the wide range of needs?
Since my first oncology massage, we’ve worked with patients with even lower platelet counts, so the bottom line is – you can work with anyone, it’s about how to adjust. If they have a platelet count of two, you’re doing gentle touch, or you’re just “lotioning” them with no pressure. If they’ve just finished their treatment, they’re still going to be fatigued, and they may have some skin issues or have lost their hair. If they’ve had surgery, their incisions may be causing problems, and if it’s radiation, they may have some facial problems.
What are the major adjustments a massage therapist might make for a cancer patient?
About 40% of the US population at some point will have cancer, so I think that every therapist should be trained to know basic adjustments. Pressure, site, and positioning are the categories of adjustments we can make. Pressure is the biggest one.
- Pressure: Everybody learns pretty deep pressure in massage school, and you might need to dial back the pressure. There are a lot of cancer patients at risk for lymphedema from having lymph nodes removed and radiation, and they just don’t train massage therapists how to make those adjustments – like what direction should you go, what type of pressure to use.
- Site: Then there are sites that you need to avoid. They might have a catheter or have had a mastectomy. Skin problems are another issue, so the site where you can actually perform a massage is another category.
- Positioning: Finally, positioning is another important adjustment. If you had abdominal surgery, you need something under your lower legs so that your belly is not all stretched out, or maybe you need a pillow to support your head.
What is the goal of an oncology massage treatment?
One of the differences between the kind of massage we do and a sports massage is that it’s slower. Our goal is rest, not range of motion, so it’s a matter of slowing down, being mindful, and incorporating breathing. There’s something about that full-handed contact and that slow speed that is the most effective for pain. In fact, the research is really well-developed for massage as an intervention for pain and anxiety across the board.
How can massage help a cancer patient?
Although much more research needs to be done, there is data showing that massage can help with pain, sleep, quality of life, mood, depression, peripheral neuropathy, anxiety and fatigue. Fatigue is a big one because there aren’t medications for fatigue. There’s some research about immune function improvement, and people say that it improves vital signs like blood pressure, heart rate, etc.
What do patients recovering from cancer want and expect from massage?
The most common thing we encounter is that people already have an idea of what massage is – they think it should be robust; the deeper the better, and no pain no gain. But for people that are fatigued, which across the board those affected by cancer tend to be, the energy of the massage needs to match their energy. They might feel okay with a heavy massage in the moment, but quite often they don’t feel well that night or the next day.
“People in treatment for cancer want to be touched fully, with calm, confident, and loving hands. They do not want those around them walking on eggshells or touching them as if they will break. Massage therapy sessions do not have to stop for cancer treatment, they need only to be adjusted.” Excerpt from “Medicine Hands: Massage Therapy for People with Cancer,” (3rd Ed.) (2014, Findhorn Press)
Is there a simple massage technique we can do to help our loved ones?
Anyone can put lotion on somebody’s feet. People think that they need deep muscle contact for relaxation to happen, but it’s the nerves in the skin that bring relaxation. Although tight muscles can create stress (tight muscles clamp down around the vessels so you don’t get good circulation, and then that builds up lactic acid,) this is about the skin. Just by applying lotion in an area, it has a layered side effect – first, there’s relaxation, and then there’s the muscles letting go.

Gayle, lower right, at the Society for Oncology Massage Summit in 2016
Can you give us an example where simply applying lotion to the skin might be helpful?
One time I worked with a lady who had had a mastectomy. The position for mastectomy surgery is with the arm lifted above the head for 90 minutes, so for most people, it’s not the incision that’s painful – it’s actually the shoulders and the neck, from keeping their arm raised. Well, they had to take her back again into surgery because she developed a hematoma. After two surgeries in 24 hours, her neck became really sore. The nurse asked, “Is there anything you can do to help her?” Using lotion, I gently stroked her neck and the top of the shoulder. No muscle contact, just skin-to-skin connection to calm the area, and that did it. She felt a lot of relief.
I know from experience that just being in a hospital can be traumatizing. How does that factor into your work?
Medical care isn’t intentionally traumatic, but it’s traumatizing to the body and the brain, and massage can help release that trauma. People are bringing a traumatized body to us and they don’t need to be re-traumatized by a robust massage. The same is true at the end of life; they have been through a lot of medical care and they need something that feels really pleasurable to the body. I know that sounds really simple, but we just bring pleasure to the body again after unpleasant things.
What are the benefits of massage are for someone nearing the end of their life?
Massage can provide a feeling of being loved, of connection. Let’s say people are panicky, massage can help calm their breathing. A lot of patients get swelling, their feet or lower legs are really tight, they’re not moving – lots of disease processes can cause swelling -and so massage, given in the right way, can move that. It doesn’t last forever, but it gives them some relief. It can help with circulation, pain, and anxiety.
Have you used touch with any of your own loved ones nearing the end of life?
With my own mother, I just sat for a couple of hours with my hands in comfortable places, like her lower extremities. There was one leg that I could access. I think she knew I was there because she died pretty shortly after I left.
Any advice for those of us with dying loved ones?
When a loved one dies, quite often people just leave them – don’t leave, they’re not gone yet. Stay and be present, and maybe you can touch them then because you’re not holding them back. It could be really healing for the people left behind, but also probably for the soul that’s working to transition.
Any self-massage tips you might give our readers?
You can just do slow circles on the chest, or circles on the abdomen (but only if someone hasn’t just finished treatment.) Or you could use simple acupressure points. There’s one called between the thumb and index finger called large Intestine 4 in Chinese medicine, and it can be used to relieve constipation or pain. They can just sit and watch TV and just squeeze that point.
What should someone look for when hiring a professional in this setting?
Look for people who have had training in lymphatic massage, or training that includes working with cancer patients so they understand the treatment process and the adjustments. Anyone that’s trained in manual lymph drainage would be appropriate. Therapists who practice gentle modalities like Reiki and Healing Touch should also be considered. If I was a family member and I was interviewing a therapist I would share what my loved one is experiencing and ask the therapist how they would adjust for those things. If they have an intake form that’s a good sign too. You could also check out the Society For Oncology Massage for their therapist locator service.
What would you tell someone just starting their career as a massage therapist?
I would tell them to do more than just massage for a living. When you’re touching people you’re really engaging with their body, their sweat, you know chemotherapy coming off their body – and it’s not sustainable to do that for 40 hours a week. It takes a while to develop any kind of alternative practice, and I think it’s too stressful to quit everything and depend on massage only. With all that pressure, it loses the magic. The magic is super important – staying fresh.
Tell me about the message in your newest book, “Hands in Healthcare.”
This book is for massage therapists, but it would be helpful to any healthcare staff nurses, anybody who touches. I want people to know that there isn’t anyone who can’t have touch. If they have liver disease, here are the adjustments. If they’re a cardiac patient, here’s the adjustment; Parkinson’s, etc. Nobody has to be turned away! This book will arm them with the right information to work with so many different people.

Gayle MacDonald, retiring after 28 years, has left an indelible mark upon the field of oncology massage.
Thank you so much for your time and your years of service, Gayle! Good luck with all your future endeavors.

 Massage Therapy Eases Cancer Patients’ Suffering
Massage Therapy Eases Cancer Patients’ Suffering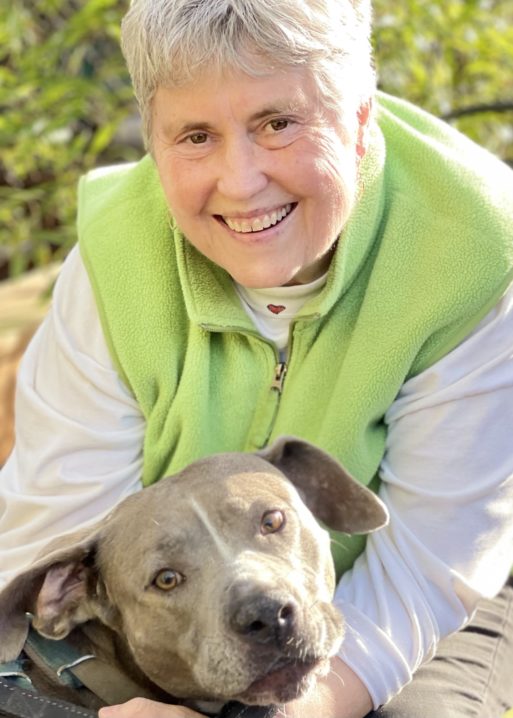



 Final Messages of the Dying
Final Messages of the Dying
 Will I Die in Pain?
Will I Die in Pain?















