Chronic pain affects up to 1.5 billion adults worldwide, leading scientists to search for new treatments.
Chronic pain can be a confusing and miserable condition for those who suffer from it and an ethical gray area for the doctors who treat it. A desire to move away from opiates and tap into a growing market for pain relief has researchers and pharmaceutical companies advancing pain medication in new directions.
Chronic pain, defined as recurring or persistent pain that lasts longer than three months, accounts for anywhere from 15% to 20% of hospital visits. Its current most common remedy is synthetic opioid analgesics, the over-prescription of which has led to a full-blown public health crisis. The ills of substance abuse and dependency have created well-documented human suffering. According to the U.S. Centers for Disease Control and Prevention, nearly 75,000 Americans died from opioid overdose in 2019 alone, and prescription opioid abuse is a major cause of suicide in U.S. citizens.
A feature in the online science and tech magazine Neo.Life outlined attempts to inhibit or rewrite genetics to block certain types of pain.
Genes like SCAN9 and proteins that are associated with sensory neurons could hold the key for future pain treatments.
Pain, Pain, Go Away
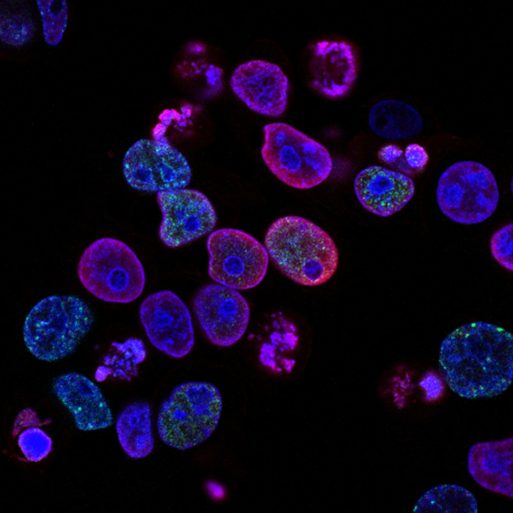
Not all people feel physical pain. Inherited congenital insensitivity to pain, a rare condition occurring in only one case per million people, presents a genetic route to chronic pain medication. Unfortunately, many people born with this condition die from untreated wounds or illnesses, making it difficult to find participants for medical research. However, scientists have found that a gene called SCAN9 may play an important role in developing insensitivity to pain. SCAN controls the production of Nav1.7 channels, which help deliver pain signals in sensory neurons. Those with a mutated SCAN9 gene develop non-functioning Nav1.7 channels and cannot register pain. Unfortunately, attempts to develop a treatment targeting Nav1.7 in the past 15 years have fallen short because the treatments also could change other similar molecules that control vital functions like muscle contraction and heartbeat rhythm.
Gene Editing Holds Promise for the Future
Scientists have looked specifically into gene editing for a finer approach to treating chronic pain. Researchers from the University of California San Diego successfully delivered a gene in mice that can code a “suppressor” protein to the SCAN9, preventing it from creating Nav1.7 channels. The treatment wouldn’t be a permanent change to the SCAN9, and instead would be “long-lasting relief,” according to Neo.Life.
Despite its success in mice, this chronic pain treatment may not see human trials for a long while since it would be an expensive process to construct a gene that would work in humans. That fact, coupled with the concerns over the effect of meddling with Nav1.7, which also plays a role in insulin secretion, could hinder the progress of a genetic solution to chronic pain.
Dentists Dive into the Past of Pain Treatments
Some methods look for inspiration from the past to devise less addictive methods of pain care. A recent literature review from the University of Michigan School of Dentistry found that naltrexone could be effective in treating chronic pain, without the same risk for addiction present in other opioids. Naltrexone was originally developed in the 1960s as an alternative to naloxone, a nasal spray used to reverse the effect of opioid drugs. Researchers found that small doses (0.1-4.5 mg) of naltrexone were able to use a unique pathway in the nervous system to calm pain signals in certain chronic pain conditions.
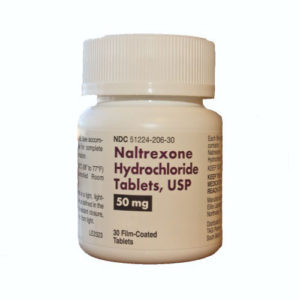
Low-dose naltrexone offers one current medical solution to certain types of chronic pain.
“Low-dose naltrexone begins to address the cause of pain and not just mask it, which allows us to better target diseases causing chronic pain, as well as potentially consider pain control outside of opioid use,” said Elizabeth Hatfield, first author and clinical lecturer at the University of Michigan.
Michigan researchers suggested that the drug was useful specifically for certain types of pain where the nervous system was in a “hyper-excited state” such as myalgia or complex regional pain syndrome.
With the myriad of chronic pain conditions, scientists and researchers are pushing research into new and old areas of pain treatment. It’s becoming clear a one-size-fits-all prescription is far from a reality, but the future of pain medication might not rest solely on bottles of opioids, which is something anyone who suffers from chronic pain can feel better about.

 Chronic Pain’s Brave New World
Chronic Pain’s Brave New World


 Final Messages of the Dying
Final Messages of the Dying
 Will I Die in Pain?
Will I Die in Pain?















