For centuries, scientists have known that the human body is host to large numbers of microorganisms. Ever since Dutch scientist Antoine van Leeuwenhoek designed his first microscope in 1666, researchers have studied the tiny creatures that populate our bodies, searching for clues about what role they play in maintaining or damaging our health.
Historically, scientists have believed that the role of most of the microorganisms that inhabit the human body was largely a protective one. Although their mechanism of action hasn’t always been clear, studies have shown that when the growth of this so-called “normal flora” is disrupted, infection-causing organisms can easily take hold.
One example: In a study cited in the textbook Medical Microbiology, investigators used the antibiotic Streptomycin to decrease the number of microorganisms in the guts of rats. They then injected the animals with streptomycin-resistant Salmonella bacteria in varying amounts. In untreated animals, it took about 10 million microorganisms to establish an infection. But in the treated mice, fewer than 10 were required to make the animals ill.
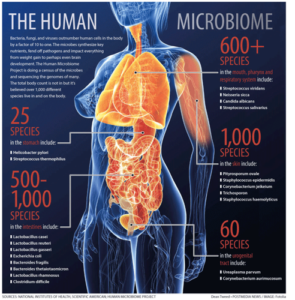
Still, studying the vast numbers of microorganisms in the human body has always been challenging, since many of them are impossible to grow in the lab. But then in the early 2000s, scientists figured out a way to sequence the DNA of the human microbiome (the term used to describe the microorganisms that live in and on our bodies, most notably in the gut). This finally gave them the key to unlocking the mystery of what each of the quadrillion-or-so microorganisms in the human microbiome do.
The Microbiome and the Brain
At first, scientists investigating the microbiome looked mostly for connections between microorganisms and the parts of the body in which they live, focusing to a great extent on gut health (hence the probiotics craze). But some scientists took their research in another direction and began looking at the possible connection between the microbiome and the brain.
Credit: nih.gov
One of these researchers is Dr. Sangram Sisodia, a neurobiologist from the University of Chicago. After listening to Dr. John Cryan present a theory about a connection between the microbiome and Alzheimer’s disease, he decided to put Cryan’s hypothesis to the test. On “a lark,” he and his colleagues fed antibiotics to mice that were genetically programmed to develop Alzheimer’s disease. Amazingly, after the antibiotics killed off much of the normal flora in the animals’ guts, the number of Alzheimer’s-related plaques and tangles in the mice’s brains decreased.
Further, when the treated mice received a fecal transplant from mice with normal microbiomes, the amount of Alzheimer’s-related protein in their brains increased.
“I never imagined it would be such a striking result,” Sisodia said. “For someone with a background in molecular biology and neuroscience, this is like going into outer space.”
The Microbiome and Behavior
Meanwhile, Dr. Sisodia wasn’t the only scientist who was looking at the link between the microbiome and the brain. Other investigators have also been searching for clues, and their work has provided some tantalizing hints about possible connections between the microbiome and behavior.
In one study, Dr. Rob Knight from the University of California took stool from mice that had been genetically altered to have voracious appetites and gain weight. Then he implanted that stool in mice that had been raised without gut microbiomes — a procedure called a “fecal transplant.” After the transplant, the “germ-free” mice developed increased appetites and became obese.
In similar experiments, Dr. Cryan found that mice raised without a gut microbiome were less social than other mice. Further studies revealed that those germ-free mice had changes in a part of their brain known as the amygdala, which is important in determining social behavior. Still other studies showed that normal mice who received a fecal transplant from humans with major depression became more passive when exposed to noxious stimuli.
Other investigators have shown similar connections between the microbiome and human neurological health. For example, studies have shown that children with autism have different microbiomes from neurotypical children, and adults with chronic schizophrenia have changes in their microbiomes as well.
What all this means for human neurobiology remains to be seen. But Dr. Sisodia is convinced that the connection is real. “We’re extremely confident that it’s the bacteria that’s driving this,” he said.
Narrowing Down Cause and Effect
Still, researchers still face a huge roadblock — how to determine which of the trillions of microorganisms in the microbiome are actually causing the changes they see. But it’s a challenge that some researchers have begun to address. In one series of experiments, Dr. Mauro Costa-Mattoli of the Baylor College of Medicine studied mice who displayed behaviors such as obsessive grooming and avoiding social interaction — both consistent with autism. Some of the mice had a genetic mutation that caused the behavioral changes, while others had been born to mothers who were fed a high-fat diet, which has been shown to have a similar effect.
When the researchers looked at the microbiome of both strains of mice, they discovered that they were missing a common microorganism, Lactobacillus reuteri. When they added that organism into their diets, the animals socialized like normal mice again.

Dr. Mauro Costa-Mattoli
Credit: bcm.edu
In the next phase of the research, Costa-Mattioli tired to determine how L. reuteri caused this result. What he found was that the bacteria release chemicals that stimulate nerve endings in the intestines, which in turn signal the vagus nerve. The vagus nerve then carries these impulses up to the brain where they cause an increase in production of the hormone oxytocin. Also known as the “cuddle hormone,” oxytocin promotes and reinforces social bonds.
Other researchers have found similar links between bacteria and neurological conditions such as epilepsy and Parkinson’s disease.
Still, scientists in the field of microbiology warn that these findings, while exciting, are very preliminary. Most researchers in the field are still working with fecal transplants in germ-free mice, which means there’s no way they can differentiate which bacteria are causing which result. And even when an organism has been identified, as in the case of L. reuteri, there are many steps that need to happen before it can be used in clinical trials.
Meanwhile, the scientific community is warning the public to take all of this research with a grain of salt. Because probiotics are available without a prescription, it would be easy for less-than-ethical companies to market probiotics as “miracle cures” (which to some extent they already have).
“The science can get mixed up with what the pseudoscientists are doing,” said Dr. Elaine Hsiao, a microbiologist at the University of California. So for now, she advises, the best approach is to wait and see.

 Scientists Are Studying the Link Between the Microbiome and Dementia
Scientists Are Studying the Link Between the Microbiome and Dementia




 Final Messages of the Dying
Final Messages of the Dying
 Will I Die in Pain?
Will I Die in Pain?















