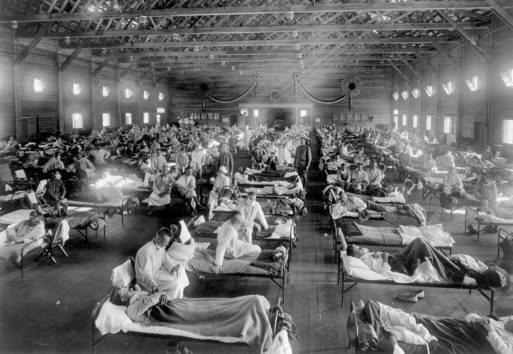
Victims of the Spanish Flu in 1918
Credit: AP Photo/National Museum of Health
At least every couple of years it seems there’s a big news story about some sort of exotic virus making the rounds far across the globe somewhere. We hear about awful things like Ebola and Bird Flu spreading in other counties, but most of us don’t think twice about it unless we have travel plans. That is until the unthinkable happens. That’s what happened in 2014, when Ebola, a disease discovered in 1976, made its first documented appearance in the United States in Dallas’ Presbyterian Hospital.
What I remember about those events is uncertainty. Could Ebola escape the confines of whatever facilities we had for such cases? If so, how does it spread? Also, what exactly is Ebola in the first place? It turns out this uncertainty is common in our healthcare system and throughout the world.
We’re Not Ready for Another Spanish Flu
The last time we experienced a global pandemic was in 1918 when a strain of H1N1 influenza (if that sounds familiar, it’s because you probably recall stories of Bird Flu outbreaks) killed as many as 100 million people worldwide. That’s as much as five percent of the world’s population at the time, and more dead than both world wars combined.
You might say to yourself, “That was 100 years ago. Surely modern medicine will protect me.” The fact is, we’re not ready for another pandemic.
The world is a different place than it was 100 years ago. The global population is almost 400 percent what it was in 1918; more than half the humans on the planet now live in cities, and travel is easier and faster than at any point in human history. This means disease can now spread more easily than ever before, and there are lots of potential pandemics waiting to hitch a ride.

Pandemics and Collective Forgetfulness
We also have a very short memory when it comes to epidemics. When Ebola first surfaced, the relatively small outbreak was contained and Ebola simply disappeared for 20 years. When it reappeared in 1995, it was misdiagnosed as shigellosis — a diarrheal disease caused by bacteria – and as a result, the death toll was much higher than it should have been before the outbreak was contained.
We have the same problem here in the United States, which translates to a lack of funding for infectious disease prevention. President Trump made a proposal in 2018 to defund the Global Health Security Agenda (a worldwide initiative begun in 2014 to help curb the spread of infectious diseases) by more than 60 percent after only four years up and running, a move that would prompt the Centers for Disease Control to drastically scale down its worldwide operations. Oh, how soon we forget.
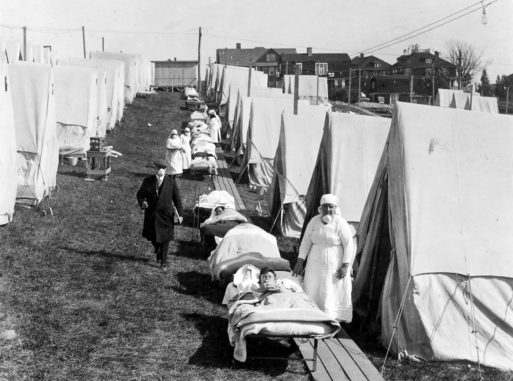
Emergency hospital in Massachusetts in 1918 for influenza cases.
Credit: National Archives
Even America Isn’t Safe
Most important, and most disturbing, is the fact that our healthcare system just isn’t prepared for another 1918 flu. It’s an economy where investment is always just-in-time, which often means a bit later than optimum. It’s also a little upsetting that our medical supply lines are precariously thin. We saw a good example of this after Hurricane Maria devastated Puerto Rico, the place where most of our intravenous saline bags are manufactured. This led to a shortage, and when medical professionals used syringes to administer fluids in the place of these bags, it led to a shortage of syringes during an especially bad flu season.
And it’s not just equipment that’s in short supply. The number of drugs deemed by the FDA to be in short supply is alarming, and every year we’re on the brink of vaccine shortages that would be catastrophic should the worst occur. Another interesting fact about these supply lines — many of them go through places like China and India, and would likely be disrupted in any sort of global crisis. Add to this the fact that it’s incredibly difficult to change anything in our hospitals in any sweeping way (they’re already almost at maximum capacity), and we’re just waiting for the other shoe to drop.
So no, we’re not ready, but we had better get ready because it’s only a matter of when we’ll see the next Spanish Flu — not if.

 Are We Ready for the Next Pandemic?
Are We Ready for the Next Pandemic?


 Final Messages of the Dying
Final Messages of the Dying
 Will I Die in Pain?
Will I Die in Pain?















