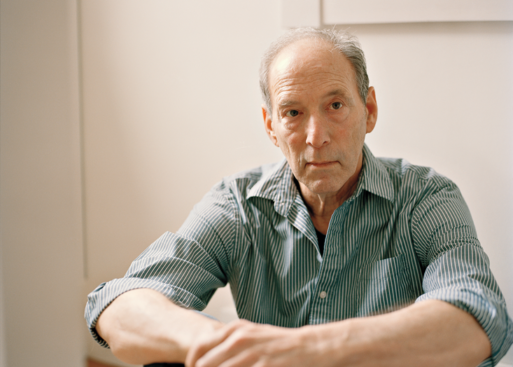
Jack Gernsheimer
Credit: nautil.us
In a small town in Pennsylvania, two identical twin brothers live almost identical lives. Jack and Jeff Gernsheimer are 68 years old. They have lived in close proximity to each other for most of their almost seven decades on earth. And since 1971, they have worked together in the same office at a graphics design company they both own. Plus, like all identical twins, they share the same DNA.
Yet Jack Gernsheimer has Parkinson’s disease, and his brother does not. And scientists at the New York Stem Cell Foundation are trying to determine why.
Genetics Versus Environment
Parkinson’s disease is associated with a number of genetic mutations, including an abnormality in the GBA and UCHL1 genes. But Parkinson’s disease is not usually hereditary. According to a 2015 article in Nautilus magazine, it’s rare even for identical twins to both have the disease. In fact, in about 89 percent of cases where one twin has Parkinson’s disease, the other one does not.
So scientists have looked at other factors in an effort to learn what sparks the neurological changes associated with Parkinson’s disease. And, as in most diseases where genes alone are not to blame, they begin by looking at environment. Research shows, for example, that Parkinson’s disease is more common in people who were prisoners of war in World War II and those who drink well water and/or live on farms. But the exact nature of the exposures that cause this to be true is unclear.

Jack and Jeff still work together every day
Credit: nautil.us
Yet it appears that environment was of little consequence in Jack’s case. After all, he and Jeff have lived and worked side by side for many years. In fact, their lives took slightly divergent courses only twice: once when they went to different colleges and again when Jack spent two years in the military.
But there is another significant difference between Jack and Jeff’s lives, and it’s one that the brothers believe may be the key to why Jack is ill and Jeff is not. In 1987, Jack’s 14-year-old son Gabriel inexplicably killed himself in a real-life reenactment of a game of Russian Roulette he had seen in the movie “The Deer Hunter.” Jack had rented the movie for the boy so he could learn more about the Vietnam war. He was also the owner of the gun.
Grief, Stress and Illness
The connection between stress and the immune system is well established. Among other things, cortisol, which is produced by the adrenal glands in response to stress, suppresses the body’s natural inflammatory response. But when stress becomes chronic, excess cortisol actually promotes inflammation by increasing the production of pro-inflammatory proteins called cytokines. These proteins are implicated in a host of autoimmune diseases, including rheumatoid arthritis and psoriasis. And scientists theorize that chronic inflammation may be a factor in the development of degenerative neurological conditions such as Parkinson’s and Alzheimer’s diseases and stroke.
Grief, of course, is immensely stressful, especially grief associated with the traumatic loss of a child. Thus, it’s not unreasonable to suspect that Jack’s grief in response to his devastating loss has something to do with his poor health. (Jack also has prostate cancer, glaucoma and psoriasis.)

Researchers grow brain cells derived from Jack and Jeff’s stem cells in the lab
Credit: anilitica.com
Searching for Clues
Researchers at the New York Stem Cell Foundation have been studying Jeff and Jack’s genome for clues as to how the brother’s differ for years. Somewhat amazingly, early on in their research they learned that Jeff has the same genetic mutation on the GBA gene as Jack. And both brothers’ brain cells (grown in cultures in the lab) produce three times the normal amount of the enzyme alpha-synuclein, which scientists believe contributes to the symptoms of Parkinson’s disease. Yet Jeff is completely without symptoms of the illness, while Jack is seriously ill.
One theory about what led to Jack’s profoundly altered health is his “experiential environment” — the emotional turmoil created by the loss of his son. According to researcher Michael Zigmond, stressful events early in life may set up the dopamine- producing cells in brain to be more vulnerable to the effects of insults later in life. Zigmond calls this effect neuroendangerment.
Molecular Changes
Another theory is that changes at the molecular level play a role in the development of Parkinson’s disease. This idea is supported by another of NYSCF’s findings: Jack’s cells have abnormally high levels of an enzyme known as MAO-B (monoamine oxidase B), while Jeff’s do not. This is important because MAO-B, which is linked to oxidative stress, is responsible for breaking down dopamine. And a loss of dopamine is what causes most of the symptoms of Parkinson’s disease.
The good news about this finding is that a class of drugs known as MAO-inhibitors already exists. And when researchers introduced one of these drugs, Rasagiline, into Jack’s cell culture, the amount of MAO-B in the cells went down and the amount of dopamine they produced went up.
Unfortunately, it’s too soon to say whether Rasagiline will benefit Jack since research into the risks and benefits of the drug has been inconclusive to date. Nonetheless, both brothers are determined to keep searching for answers to the mysterious origins of Jack’s disease. But, they are also realistic. As Jeff said to Nautilus, “Unfortunately, there’s a fair amount of testing still to be done.”

 Can Grief Contribute to Parkinson’s Disease?
Can Grief Contribute to Parkinson’s Disease?


 Final Messages of the Dying
Final Messages of the Dying
 Will I Die in Pain?
Will I Die in Pain?















