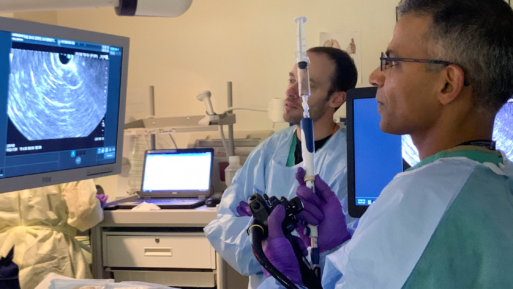
Somashekar Krishna, MD, and his team at OSUCCC-James
explore a patient’s pancreas with a “virtual biopsy.”
Credit: The James Multimedia Newsroom
Although there is much debate regarding Artificial Intelligence (AI) – the ethics, reliability and lack of oversight or guardrails for its usage – the medical field has found one way in which AI is proving to be a boon without major drawbacks: helping physicians identify and diagnose cancer and pre-cancerous growths.
Pancreatic Cancer: The Silent Killer
Pancreatic cancer is often referred to as “the silent killer” because detection and diagnosis are extremely difficult. With no associated tell-tale early warning signs or symptoms, the disease often goes undetected until it is too late. According to the American Cancer Society, the survival rate for all stages of pancreatic cancer combined is only 13% after five years. This dismal rate is due to the fact that about 80% of patients are only diagnosed after the disease has reached an advanced stage, affecting other organs that in turn cause symptoms that raise a red flag. Unfortunately, the longer cancer progresses unchecked, the harder it is to treat or cure.
According to the Hirshberg Foundation for Pancreatic Cancer Research, early detection would vastly improve the survival rate. Approximately 15-20% of pancreatic tumors can be surgically removed; if found before metastasis, these tumors show better patient survival rates.
The OSUCC – James Study on AI and Pancreatic Cancer Identification
While AI is not commonly used in cancer diagnoses, doctors and researchers are developing ways to deploy AI to help them determine what might be cancer, predict what might develop into cancer, and devise personalized treatment plans when cancer is found. The advantage lies in the fact that unlike human beings, AI tools can analyze massive amounts of data – like imaging from mammograms or biopsies – to identify patterns or anomalies that would otherwise be difficult to see.
Researchers with the Ohio State University Comprehensive Cancer Center – Arthur G. James Cancer Hospital and Richard J. Solove Research Institute (OSUCCC – James) have turned to AI to help detect pancreatic cancer earlier, perhaps even in precancerous stages. They do so by using the technology to analyze pancreatic cysts, of which approximately 25% develop into cancer.
Essentially, the researchers use mini probe-based laser optical cameras in a procedure called endoscopic ultrasound to perform a “virtual biopsy,” providing a detailed, microscopic view of the cyst wall. The problem then lies in how to accurately analyze the data in order to identify cancer risk factors. Dr. Somashekar Krishna, gastroenterologist and researcher with the program, compares it to “asking someone to count all the black, white and blue cars in a video where the cars are moving at 100 mph. It’s simply impossible without slowing down the video and analyzing hundreds, if not thousands, of individual frames.”

Dr. Krishna reviews video of a patient’s pancreas.
Credit: The James Multimedia Newsroom
The solution they’ve devised is to work with OSUCCC – James’s computer science engineers to develop and train an AI algorithm, which can analyze video from inside the pancreas to determine whether a cyst may develop into cancer. Their hope is that this AI tool can be used to identify cancer risk factors amongst hundreds of fast-moving video images in a matter of seconds, rather than hundreds of hours of laborious (and inexact) human effort.
The Potential Impact of AI in Cancer Identification
By utilizing AI to analyze the data obtained from the minimally invasive procedure, physicians can avoid other, more invasive procedures like biopsies or surgery. In the case of pancreatic cancer, it could lead to far more positive outcomes by allowing physicians to identify the disease before it gets the chance to progress. It can also reduce the time patients are left anxiously waiting for results from those procedures.
For example, one article from the Association of American Medical Colleges (AAMC) tells the story of a woman who noticed a “worrying lump” in her thyroid that wouldn’t go away. Her doctor ordered an ultrasound exam, and the results were concerning enough that a biopsy was done to see if the lump was cancerous. The patient then sought a second opinion from a radiologist who does thyroid ultrasound exams using AI. By providing a more detailed image and analysis, the radiologist was able to conclude that the tissue was benign – the same conclusion reached by the pathologist who studied her biopsy tissue. “I’m an example of a patient who had a biopsy that could have been prevented by using AI,” said the patient, who “suffered weeks of anxiety and lost sleep while awaiting the final results from her doctor.”
The researchers associated with the OSUCC – James study are hopeful that AI can prove to be a powerful diagnostic tool for the early detection of pancreatic cancers, paving the way for other similar treatments to follow.

 How Artificial Intelligence Is Being Used to Help Physicians Identify Cancer Earlier
How Artificial Intelligence Is Being Used to Help Physicians Identify Cancer Earlier


 Final Messages of the Dying
Final Messages of the Dying
 Will I Die in Pain?
Will I Die in Pain?















