Pain psychologist and mindfulness expert Leslie Aria, Ph.D., explains how people with life-limiting illnesses and other forms of chronic pain can find relief
Leslie Aria, Ph.D., teaches patients to use meditation and mindfulness techniques to manage pain.
Mindfulness has become a hot topic in recent years. From apps and podcasts to K–12 mindfulness schools and accredited mindfulness teaching programs, it’s clear that the benefits of mindfulness have a strong appeal in today’s world. This is especially true for those dealing with life-limiting illnesses and the elderly, who often suffer from significant pain. Research shows that practicing mindfulness can actually reduce the experience of physical suffering. Leslie Aria, Ph.D., has been helping his patients do just that for 16 years.
Aria is a pain psychologist at Kaiser Permanente in Sacramento, California. When he first started out as a psychologist, he told himself he would never work with chronic pain patients. “I was afraid,” he said. But during his graduate work, he became fascinated with the relationship between medical conditions and depression — how one often led to the other, and vice versa. Now, he helps patients with chronic pain utilize mindfulness and meditation techniques to manage their pain.
Earlier this year, Aria started Myndfulness, a website with free meditation resources and information. When COVID-19 hit California in March, he started getting emails from patients who could no longer afford to see him because they’d lost their jobs and insurance. He saw a need for free, accessible resources for people looking to try mindfulness techniques or continue their practice. He is also the co-founder of RemedyPain.co, and in January 2021, he will also be hosting the first Solving Chronic Pain Summit with Dr. David Clawson, Dr. David Hanscom and Stephen Porges, Ph.D.
Editor’s Note: This interview has been edited for length and clarity.
Thank you so much for joining us today. To start us off, would you mind explaining what pain psychology is — and how you started working in the field?
A pain psychologist specializes in treating persistent pain — whether that’s headaches, migraines, neck pain, back pain, IBS or even post-chemotherapy pain. I use the term “persistent pain” because “chronic pain” is used so much that there’s a certain ambivalence toward it. When you use different terminology, it wakes the brain up a little, and we say, “What’s that?”
Pain psychologists focus not just on thoughts and feelings but the physiology behind them. When I did a rotation in the chronic pain department in grad school, I saw the provider struggle with the patients — they were angry because nothing was working, and they wanted more opioids. They were really suffering, and I thought, “I don’t want to be part of this.” I didn’t truly understand why they were angry. But eventually, I found good mentors who asked me, “Wouldn’t you be angry if you were in chronic pain and couldn’t get out of it?” When I started to understand that, I wasn’t afraid to help the patients anymore. I ended up getting additional training, and now — I love my work. I’m so blessed to be able to help people who are suffering and actually hold space for them — and change their physiology.
Are patients usually open to the idea of managing pain through mindfulness, or do you find there’s some resistance to it?
A lot of patients see me as their “last stop” when everything else has failed. They may have tried medical treatments or acupuncture and found it didn’t work for them. Sometimes their reaction to the idea of mindfulness is, “But this isn’t just in my head.” Ironically, it is in their head, in a sense — in their brain — but I let them know that I’m not going to try to dissuade them.
I start by asking patients what the most taxing thing for them is — say, if they have lower back pain — and I ask them, “If I can shift your pain in today’s visit, would you be open to seeing me again?” Often, they say, “You’re on. What have you got?”
Let’s talk a bit more about what mindfulness is. Is it the same as meditation?
There’s formal mindfulness, which is meditation — setting aside time to practice mindfulness with a specific focus, like breath. There is over 35 years’ worth of research showing that meditation helps balance your nervous system. Then there’s informal mindfulness, which has to do with where you focus your attention as you’re going through your daily activities. When you drink a sip of your tea, are you just drinking tea, or are you drinking tea and worry? When you take a shower, are you by yourself, or are you with all the people and problems in your head?

Aria helps patients manage their pain to engage in daily activities again.
Informal mindfulness involves engaging all five senses. For instance, I’m drinking this tea, and it smells like rose. It’s warm, and I can feel my fingertips getting warm. I can hear it swishing in the glass. That’s an example of informal mindfulness. Doing this will train you to be aware during difficult moments when you’re feeling pain. It trains you to wake up from what’s dominating your brain in that moment.
Mindfulness helps you focus on what I call the three As. The first is attention. Your attention is your currency — if your attention is on the past, that leads to feelings of depression. If your attention is on the future, that leads to anxiety. Next, you have to build awareness of what’s going on inside, what’s pushing you around — your inner critic. Then you work on changing your attitude — fostering qualities that are helpful, like curiosity, non-judgment and kindness.
Can mindfulness be helpful for those with life-limiting illnesses?
A daily mindfulness practice helps reduce unnecessary suffering by helping us cultivate awareness when we are hooked by our internal storylines. Mindfulness also helps us develop helpful mental qualities such as kindness, acceptance, non-judgment, and curiosity. It helps us conserve and appreciate each present moment.
In my work, I’ve experienced a spectrum of terminal illness and end of life issues with patients and family members. I recall one patient who was suffering greatly from a terminal illness and shared with me that he had not spoken to his sons in 30 years. After practicing mindfulness for two weeks, he decided to reach out to his sons and ask for their forgiveness. He was able to pass with love, not shame.
Training ourselves to focus in the present moment and to stop struggling with our reality can lead to less suffering. The most common report I get from patients is, “I feel more peaceful; more loving and accepting of myself, especially when I am scared at night.” Mindfulness takes the sting out of our suffering.
What is the science behind chronic pain and managing pain through mindfulness?
Chronic pain is no longer about structure, nerves, and tissue damage. That’s old science. Newer science shows that chronic pain occurs because the nervous system continues to be on the defense.
Research has shown that practicing mindfulness regularly — say, for about 20 minutes a day for eight weeks — actually shrinks the amygdala, or the part of our brain responsible for strong emotional reactivity. We become less reactive when negative thoughts occur, and we identify less with strong negative emotions. That, in itself, reduces physical sensation.
We think of the benefits of mindfulness as being intangible, but in some ways they are very concrete and measurable. For instance, I can tell whether patients have been practicing mindfulness by measuring something called their heart rate variability. When your HRV is on the higher side, it shows that you are taking care of yourself, you’re open to the stressors of the day. A low HRV is associated with psychological rigidity, and when you have low HRV you’re more vulnerable to illness. Your immune system is compromised. Looking at a patient’s HRV is a bit like looking at blood work for a diabetic.
What are some of the techniques you might use with a first-time patient to begin managing pain through mindfulness?
My approach has three steps: Re-educating the patient, helping them retrain their nervous system, and re-engaging them in life. All the things they said they couldn’t do — we work on getting them back to doing those things.
One thing I’ll do with new patients is have them put their hands on their belly and ask them to focus on their thumb. When they breathe in, they raise their thumb up; when they breathe out, they lower it down. They repeat this for each finger, three times. At the end, they tell me that yes, their pain shifted during the exercise — but now it’s back. I ask them, “Where did your pain go during that time?” It was nowhere to be found. Now the key is to stretch that out. We’re reorganizing the nervous system into a more healthy state.

Aria practices mindfulness techniques throughout the day.
Patients often tell me they don’t have time to practice mindfulness, so I ask them, “Do you have one minute and five seconds?” That’s how long it takes to do the breathing exercise with your hands on your belly. I do little mindfulness practices like that throughout the day. I meditate for a total of about two hours every day — in the morning for 20 minutes, and then sprinkled throughout the day in these smaller moments.
Thank you so much for talking with us about managing pain through mindfulness today. It’s been a pleasure to speak with you.



 Nursing Home Staff Find Creative Ways to Make Holidays Fun for Residents on Lockdown
Nursing Home Staff Find Creative Ways to Make Holidays Fun for Residents on Lockdown A Moving Quote About Taking Time to Grieve from Catherine Sanders
A Moving Quote About Taking Time to Grieve from Catherine Sanders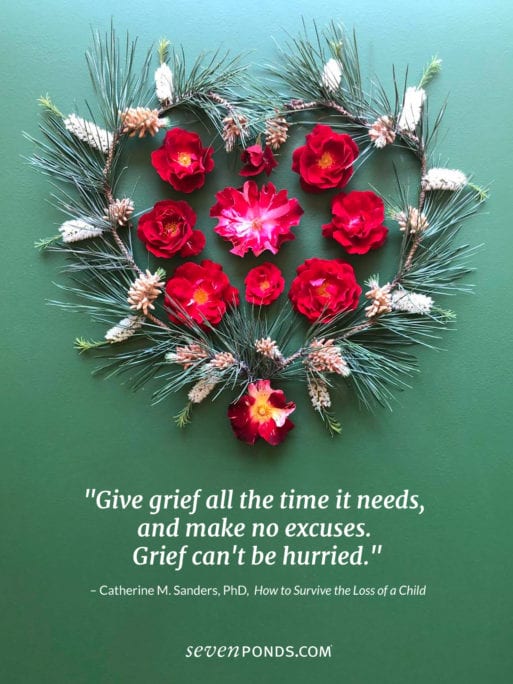
 “Dick Johnson is Dead” Directed by Kirsten Johnson
“Dick Johnson is Dead” Directed by Kirsten Johnson In the Netflix film “Dick Johnson is Dead,” documentary filmmaker
In the Netflix film “Dick Johnson is Dead,” documentary filmmaker 
 Managing Pain Through Mindfulness and Why It Works
Managing Pain Through Mindfulness and Why It Works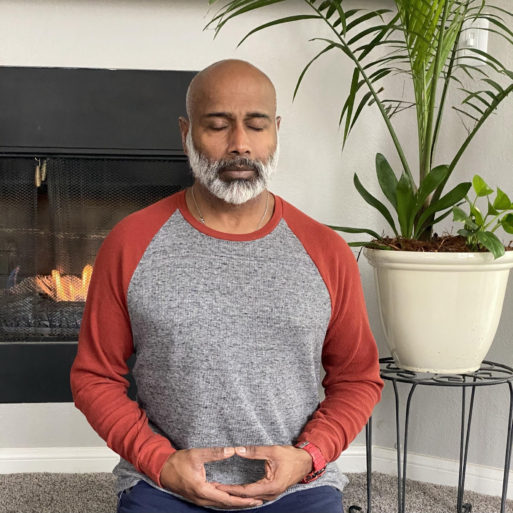


 Christmas Lights Bring Hope and Cheer Amid Pandemic
Christmas Lights Bring Hope and Cheer Amid Pandemic










 Rutgers Health Study May Improve End-of-Life Care
Rutgers Health Study May Improve End-of-Life Care
 Mary Oliver’s “Heavy” Speaks to the Weight of Grief
Mary Oliver’s “Heavy” Speaks to the Weight of Grief















