
Credit: BBC.
Filmmaker Paul Myles’s short film for BBC News about end-of-life care during the COVID-19 crisis asks five doctors working during the COVID-19 crisis the question: “How has coronavirus changed how doctors deal with and feel about death?”
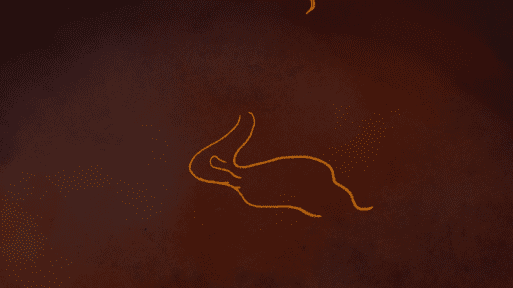
The film opens with voice-overs from the doctors’ interviews over serene, hand-drawn 2D animation by May Kindred-Boothby. Doctors relay anecdotes about the ways in which people typically spend meaningful last moments with loved ones in hospice before they die: reading their loved one a poem, sharing some wine, simply being a familiar presence in the room. Because, as Dr. Rosie Chester says in the film:
“Even if someone is unconscious or confused, they may recognize a tone of voice, perfume, the touch of a hand.”
The languid, ethereal vibe of the film abruptly transitions with a voice-over narration of a reporter informing the British public that the Foreign Secretary has said that the lock-down across the U.K. will remain in place for now, since the U.K. has not yet reached the peak of the virus.
Then we move back to doctor interviews, with physicians speaking about their real-time experiences with end-of-life care during the COVID-19 crisis. Dr. Leo Trinik tells us that before COVID-19, he would get called to look at one or two deaths in a night, “whereas now, it seems like there are often 10 people dying each night in the hospital.”
Credit: BBC.com
Dr. Arash Saleh, respiratory registrar, describes having to look after patients actively dying from COVID-19 who couldn’t see the faces of anyone who was looking after them, including himself.
Dr. Saleh also relates an incident in which he entered a hospital room, and the patient’s phone was ringing. Rather than address the ringing phone, Dr. Saleh and his team moved on to focusing on the patient’s medical care and trying to optimize his oxygen. The patient died the following morning. Dr. Selah worried afterward, wondering if there was something he could have done to make sure the patient could have spoken with his wife one last time.
Dr. Silas Webb reports that in his hospital there is now a blanket rule banning family members from visiting the intensive care department. People have also been banned from entering the mortuary with their loved one’s body because of infection control measures. Dr. Webb says:
“I think there’s going to be a huge amount of emotional trauma like that that comes out of COVID-19 because people aren’t really able to process the death of their loved ones right now.”
Credit: BBC News
May Kindred-Boothby’s hand-drawn animation
“Some of the staff are struggling, coming in and finding that out that of their list of 10 or 15 patients, there’s only two alive after literally only one night,” reports palliative medicine registrar Dr. Rosie Chester. She explains that there is a real issue in palliative medicine with emotional burnout. But Dr. Chester and her colleagues are doing what they can to give people as comfortable and as normal a death as possible. Healthcare workers, just like everyone else dealing with the pandemic, are learning as they go.
Dr. Webb concludes with a statement about the U.K.’s resistance to talking about death (similar to the reticence to discuss death in the United States). He says:
“Potentially, something that this awful pandemic will do is making people much more aware of their mortality and making it much more acceptable to be talking about.”
If there’s any good that comes out of this global crisis, let one of them be more open discussion about the biggest transition any of us will ever make.

 “End-of-Life Care During the COVID-19” Crisis by Paul Myles
“End-of-Life Care During the COVID-19” Crisis by Paul Myles


 Final Messages of the Dying
Final Messages of the Dying
 Will I Die in Pain?
Will I Die in Pain?















